Proposal of collaboration
Validation of a classification system for a better prognostic stratification of recurrent thymic epithelial tumor patients
Introduction
 We have recently published the following manuscript in JTO: Chiappetta M, Lococo F, Zanfrini E, Moroni R, Aprile V, Guerrera F, Nachira D, Congedo MT, Ambrogi MC, Korasidis S, Lucchi M, Filosso PL, Ruffini E, Sperduti I, Meacci E, Margaritora S. The International Thymic Malignancy Interest Group Classification of Thymoma Recurrence: Survival Analysis and Perspectives. J Thorac Oncol. 2021 Nov;16(11):1936-1945 (to read the article CLICK HERE – log on JTO website is required).
We have recently published the following manuscript in JTO: Chiappetta M, Lococo F, Zanfrini E, Moroni R, Aprile V, Guerrera F, Nachira D, Congedo MT, Ambrogi MC, Korasidis S, Lucchi M, Filosso PL, Ruffini E, Sperduti I, Meacci E, Margaritora S. The International Thymic Malignancy Interest Group Classification of Thymoma Recurrence: Survival Analysis and Perspectives. J Thorac Oncol. 2021 Nov;16(11):1936-1945 (to read the article CLICK HERE – log on JTO website is required).
We retrospectively collected data on 135 patients treated surgically for recurrent thymomas at three Italian high-volume centers. Recurrences were classified according to the ITMIG classification as:
- local
- regional
- and distant.
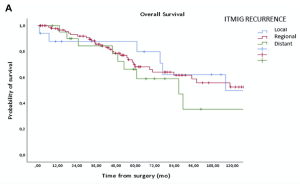
In the analysis presented here, the ITMIG classification and an alternative classification taking into account other clinico-pathological variables were correlated with overall survival (OS). According to our data, the 5- and 10-year OS were 79.9% and 49.7% in local, 68.3% and 52.6% in regional, and 66.3% and 35.4% in distant recurrences, respectively, but differences were not statistically significant (p = 0.625).
Interestingly, a significant difference in survival was observed when comparing single or multiple sites of recurrence: 5- and 10-year OS of 86.2% and 81.2% versus 61.3% and 31.5% (p = 0.005, hazard ratio = 7.22, 95%, confidence interval: 0.147–0.740), respectively.
Thus, we combined the number of recurrence (“single” vs “multiple”) with the site of recurrence (local + regional vs. distant) noting that loco-regional single recurrence had a statistically significant better survival compared to patients with ITMIG loco-regional multiple recurrence or ITMIG distant recurrence (p =0.028). Similarly, a significant difference was found between intrathoracic (loco-regional + lung metastases) single recurrence and intrathoracic multiple and distant recurrence (p = 0.024).
These two classifications proposed seem to be able to stratify prognosis in our relative large cohort of patients. However, external validation is needed to finally propose a system that is useful in daily clinical practice.
Purpose of the Project
The goal of the current international ITMIG project is to collect retrospective data on patients with TETs recurrence from various ITMIG collaborating centers (minimum 100 patients) in order to:
- perform external validation of the results obtained based on the 2 classifications for thymoma recurrence used to date
- test these two classifications (or explore another one) in all recurrent TETs (thymomas + thymic carcinomas)
- test these two classification (or explore another one) in recurrent thymic carcinoma cases only.
Methodology and Inclusion Criteria
Inclusion Criteria
- TET (thymoma, thymic carcinoma and thymic neuroendocrine tumor) patients who underwent radical resection (R0) or R1 resection (only if a proper RT treatment was performed on surgical bed) with a recurrence pathologically proven or certified by a multidisciplinary discussion. There are no restrictions on the date of resection of the primary tumor.
- No missing data in the “minimum data set” (sex, age, Masaoka-Koga stage (at thymectomy), TNM stage (at thymectomy), WHO classification (at thymectomy), R-status at thymectomy, pattern of recurrence (ITMIG classification), disease-free interval (from thymectomy to recurrence), number of recurrent tumors (single vs. multiple), site of recurrence (pleura, lung parenchyma, both, other), treatment of recurrence, R-status of recurrence treatment, follow-up information.
Additional Information
There are no restrictions on the date of resection of the primary tumor, that is, patients whose primary surgery took place many years ago can be included in the study. Imaging data are crucial at the moment of recurrence to define the pattern of relapse (i.e.: site, number).
The occurrence of a 2° relapse or the detection of tumor progression after 1° relapse have to be pathologically proven or certified by a multidisciplinary discussion.
Practical Information
A “clean” version of the Excel spreadsheet with all data that should be collected will be sent to each participant interested in joining the project. If necessary, it is possible to directly contact the data manager from our institution (Catholic University of the Sacred Heart, Rome, Italy) who is assigned to this project.
The number of CE authorization will be provided to each participant for the ethical approval (if required by local rules).
Finally, the statistical analysis will be performed by an external expert statistician that will be supervised by the P.I. (Prof. Lococo) and co-P.I. (Dr. Chiappetta, from same Institution).
Updated information about the study will be provided to all participants and results will be discussed at a dedicated meeting.
Contact
If you have any questions, please do not hesitate to contact me – CLICK HERE.
Kind regards,
Filippo Lococo
Professore Associato in Chirurgia Toracica
IRCCS-Fondazione Policlinico Gemelli, Università Cattolica del sacro Cuore, Roma, Italia