The classical surgical approach for thymic epithelial tumors is a sternotomy providing a wide access to the prevascular (anterior) mediastinum where the tumor is located. For very large tumors a so-called clamshell approach may be used to remove the tumor completely; this transverse incision extends on both sides of the chest giving broad access to the heart, mediastinum and both lungs.
 During the last decade minimally invasive approaches have been more widely used. These include video-assisted thoracic surgery (VATS) and robotic-assisted thoracic surgery (RATS). The operation is performed by several small incisions (thoracoports) reducing the amount of pain and allowing more rapid recovery, especially in patients with myasthenia gravis. Several variations of VATS and RATS exist, also depending on the specific center and the experience of the individual surgeon. Depending on the location of the tumor, a left-sided or right-sided approach is used and more recently, the operation has been performed by an incision below the sternum (subxiphoid). The robotic approach provides a magnified 3-dimensional view with highly flexible robotic arms allowing a very precise dissection. However, the cost of RATS is much higher compared to the other techniques.
During the last decade minimally invasive approaches have been more widely used. These include video-assisted thoracic surgery (VATS) and robotic-assisted thoracic surgery (RATS). The operation is performed by several small incisions (thoracoports) reducing the amount of pain and allowing more rapid recovery, especially in patients with myasthenia gravis. Several variations of VATS and RATS exist, also depending on the specific center and the experience of the individual surgeon. Depending on the location of the tumor, a left-sided or right-sided approach is used and more recently, the operation has been performed by an incision below the sternum (subxiphoid). The robotic approach provides a magnified 3-dimensional view with highly flexible robotic arms allowing a very precise dissection. However, the cost of RATS is much higher compared to the other techniques.
Minimally invasive approaches are generally used for clearly resectable tumors until 5 cm without invasion of neighbouring organs or structures.
 More about minimally invasive surgery of the thymus you can find in a special series published in Mediastinum and presented on our webpage: Minimally Invasive Thymectomy.
More about minimally invasive surgery of the thymus you can find in a special series published in Mediastinum and presented on our webpage: Minimally Invasive Thymectomy.
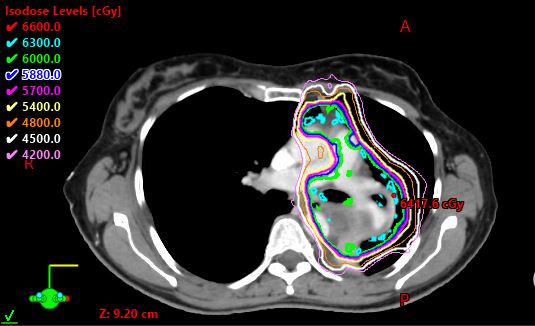
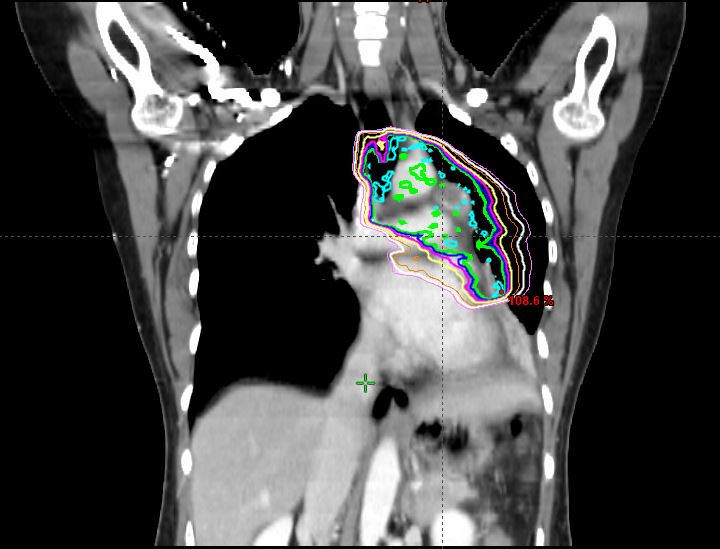
For unresectable tumors only a biopsy is taken after discussion in a multidisciplinary tumor board. This is mostly performed by a 3-4 cm incision on the left or right side of the sternum (anterior mediastinoscopy) which provides immediate access to an anteriorly located tumor allowing large incisional biopsies which are essential to provide a definite diagnosis. For these, stage III or IV tumors multimodality therapy is indicated.