Minimally Invasive Thymectomy
A big picture focus on minimally invasive thymic surgery
Frank Detterbeck
Section of Thoracic Surgery, Yale University School of Medicine, New Haven, CT, USA
This special issue of the journal Mediastinum is focused on minimally invasive surgical approaches for thymectomy. There is no question that surgery in general is being transformed from the traditional large open incisions to less invasive approaches. This is true for mediastinal disease as well, although one can argue that the published literature on this topic is well behind that on minimally invasive lobectomy or esophagectomy. This is probably due to the fact that thymic hyperplasia and tumors are much less common than lung or esophageal tumors.
The International Thymic Malignancy Interest Group (ITMIG) exists in order to promote advances in the management of patients with thymic or other mediastinal conditions. Recognizing that for rare diseases it is essential to collaborate, ITMIG has brought together a global community of people interested in these conditions. It is fitting then, that ITMIG instigated this initiative of a special issue of Mediastinum on minimally invasive surgical approaches.
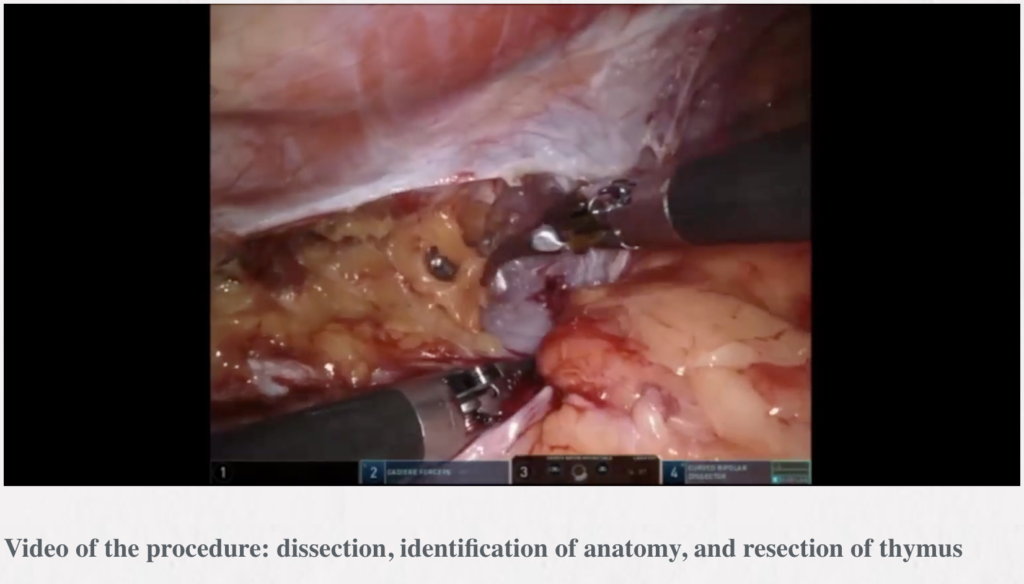
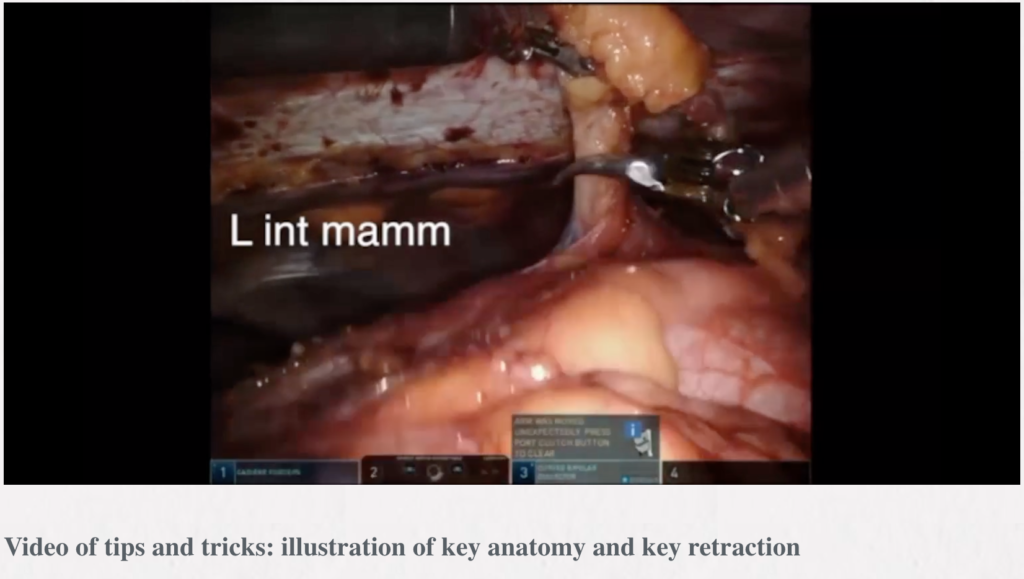
Robotic thymectomy
Timothy Mark Lee, Robert J. Cerfolio
 Subxiphoid single-port thymectomy procedure: tips and pitfalls
Subxiphoid single-port thymectomy procedure: tips and pitfalls
Takashi Suda
Department of Thoracic Surgery, Fujita Health University School of Medicine, Toyoake, Aichi, Japan
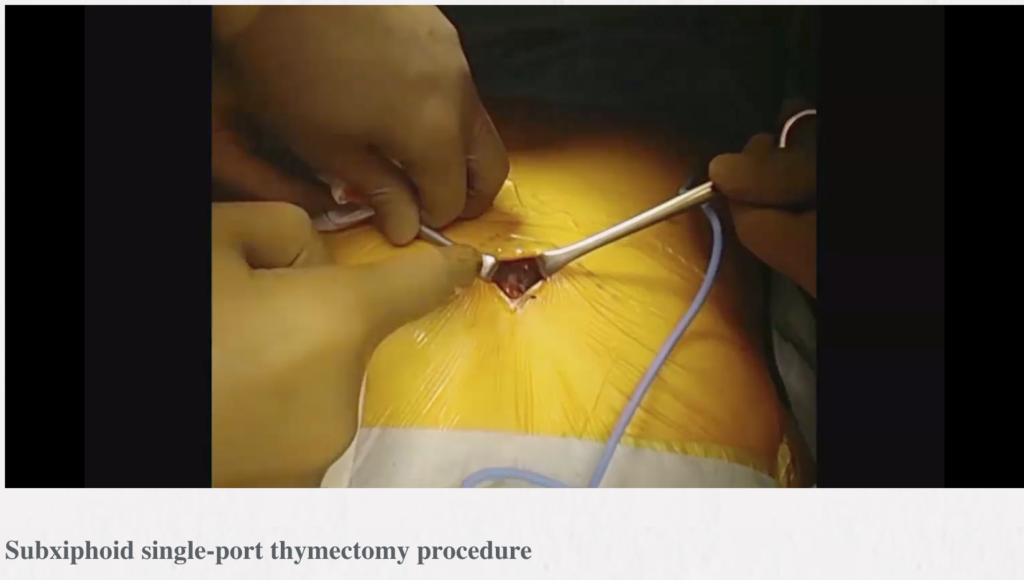
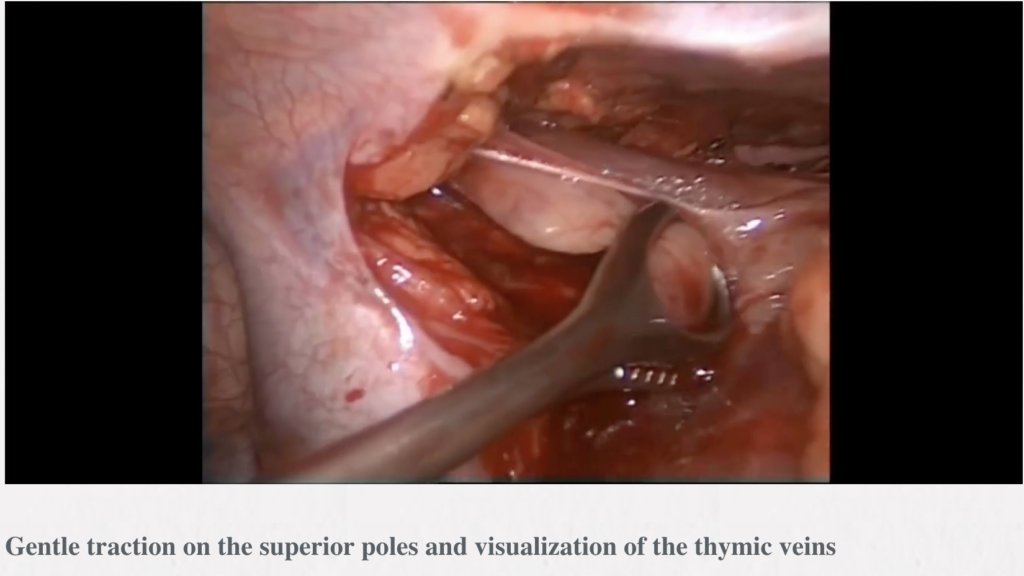
Abstract: We previously described a subxiphoid single-port thymectomy procedure with CO2 insufflation of the mediastinum and removal of the thymus via a single incision below the xiphoid process. This report describes an endoscopic subxiphoid, single-port thymectomy procedure, with tips to ensure success and pitfalls to avoid. The patient is placed in the supine position with the legs apart. A vertical or horizontal incision of approximately 3 cm is made 1 cm caudal to the xiphoid process. A finger is inserted behind the sternum via the subxiphoid wound to blindly detach the caudal side of the thymus from the sternum. A port for single-port surgery is inserted. CO2 insufflation is performed at 8 mmHg. The trick to safe use of the vessel sealing device is to perform separation by opening and closing the jaw tips before dissection, passing one of the jaws through the separated area, and then dissecting. In a subxiphoid single-port thymectomy, the thymic vein is sectioned last because it runs tangential to the subxiphoid wound and shifts laterally on the traction of the thymus. The thymus is removed from the body through the subxiphoid incision. The subxiphoid approach affords a cervical field of view that is superior to other approaches and makes it easy to identify the bilateral phrenic nerves. Furthermore, it is a minimally invasive approach that reduces the extent of intercostal nerve damage compared with the lateral intercostal approach. Thymectomy using the subxiphoid approach is a surgical technique that should be learned by respiratory surgeons.
Subxiphoid robotic thymectomy procedure: tips and pitfalls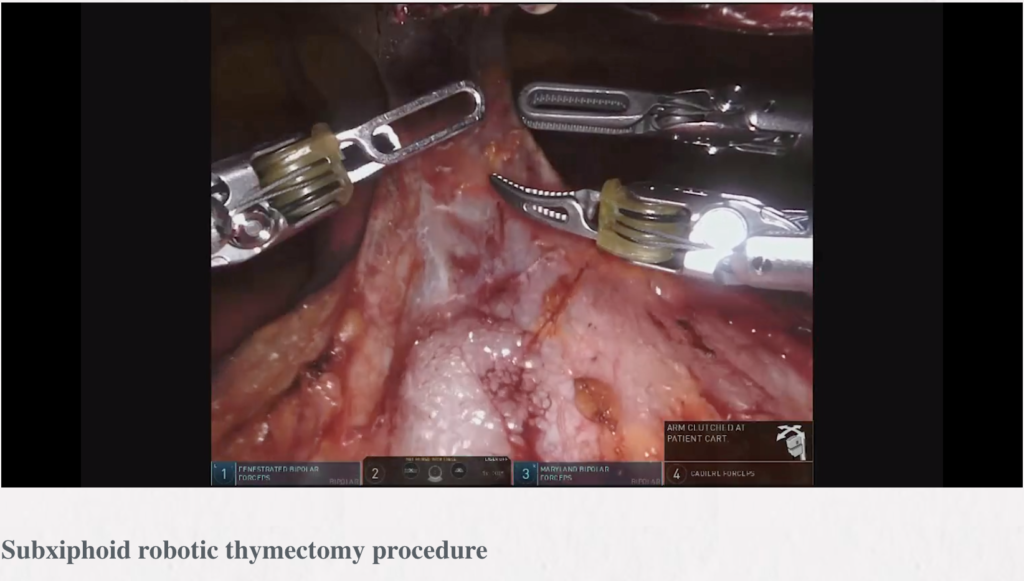
Takashi Suda
Department of Thoracic Surgery, Fujita Health University School of Medicine, Aichi, Japan
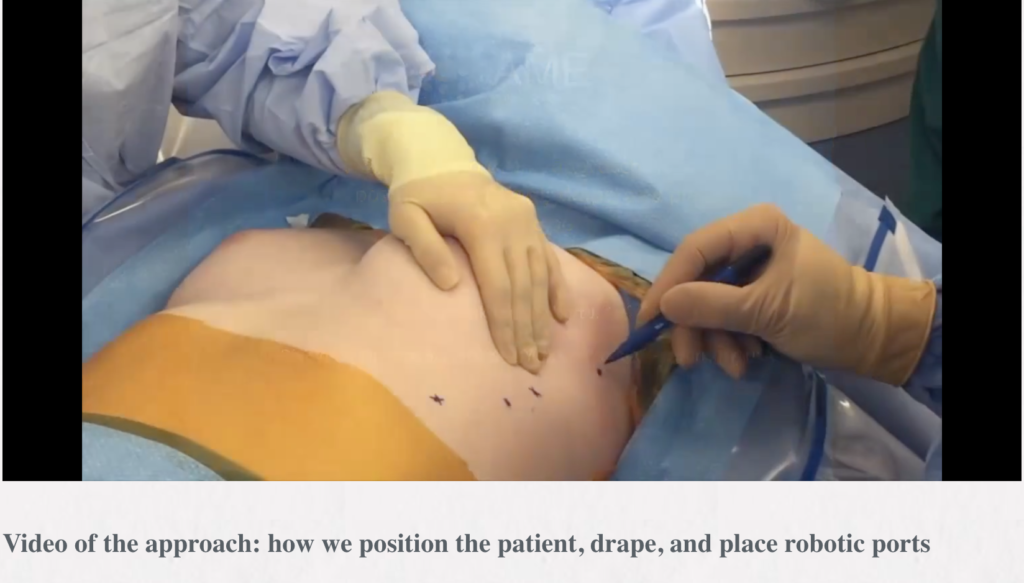
Abstract: Recently, robot-assisted surgery has gained popularity for thymectomy. The advantages of robot-assisted surgery include true three-dimensional (3D) imaging with binocular glasses and the use of multiarticular forceps that allow the performance of high-precision operations. Furthermore, the presence of devices with multiple articulations within the thoracic cavity enables detachment procedures to be achieved in a natural manner. In the subxiphoid robotic thymectomy, the camera scope was inserted through a midline subxiphoid incision, which provides an operative visual field like that obtained during median sternotomy, making it easy to identify the neck structures and the location of the bilateral phrenic nerves and to observe the entire left brachiocephalic vein. This report described the surgical indications and techniques of subxiphoid robot-assisted thymectomy (SRT). The patient is in the supine position with the arms and legs apart. A 3 cm vertical incision is made approximately 1 cm caudal to the xiphoid process. CO2 insufflation is performed at 8 mmHg. The mediastinal pleura is sectioned bilaterally to expose the thoracic cavity. A 1 cm skin incision is made along each of the bilateral anterior-axillary lines at the sixth intercostal space of the precordium to insert the port for the da Vinci system arm. When using the retraction arm, a port is inserted at least 6 cm from the port on the anterior-axillary line to the mid-axillary line in the right sixth intercostal space. Robot-assisted surgery is performed with multi-articulated forceps that move like human joints. This allows safe clamping of the left brachiocephalic vein even if it is in contact with the tumor. Subxiphoid robotic thymectomy allows for minimally invasive surgery in some patients previously considered unsuitable for thoracoscopic surgery such as in those with brachiocephalic vein involvement or with pericardial invasion requiring a more complicated surgery.
Minimally invasive resection of thymoma
Alper Toker1,2, Erkan Kaba3, Kemal Ayalp2, Tugba Cosgun3, Mazen Rasmi Alomari2
 1Department of Thoracic Surgery, Istanbul Faculty of Medicine, Istanbul University, Istanbul, Turkey; 2Department of Thoracic Surgery, Istanbul Hospital, Group Florence Nightingale Hospitals, Istanbul, Turkey; 3Department of Thoracic Surgery, Medical Faculty, Istanbul Bilim University, Istanbul, Turkey
1Department of Thoracic Surgery, Istanbul Faculty of Medicine, Istanbul University, Istanbul, Turkey; 2Department of Thoracic Surgery, Istanbul Hospital, Group Florence Nightingale Hospitals, Istanbul, Turkey; 3Department of Thoracic Surgery, Medical Faculty, Istanbul Bilim University, Istanbul, Turkey
Abstract: Minimally invasive thymoma resection is a hot debate topic in thoracic surgery. However, more than 14 techniques have been described for approaching the mediastinal region, although the type of resection should be similar in all. In this article, we aim to review the literature on thymoma operations that included minimally invasive thymoma resection. In addition, we share both our clinical experience and surgical techniques, mainly including VATS and robotics.
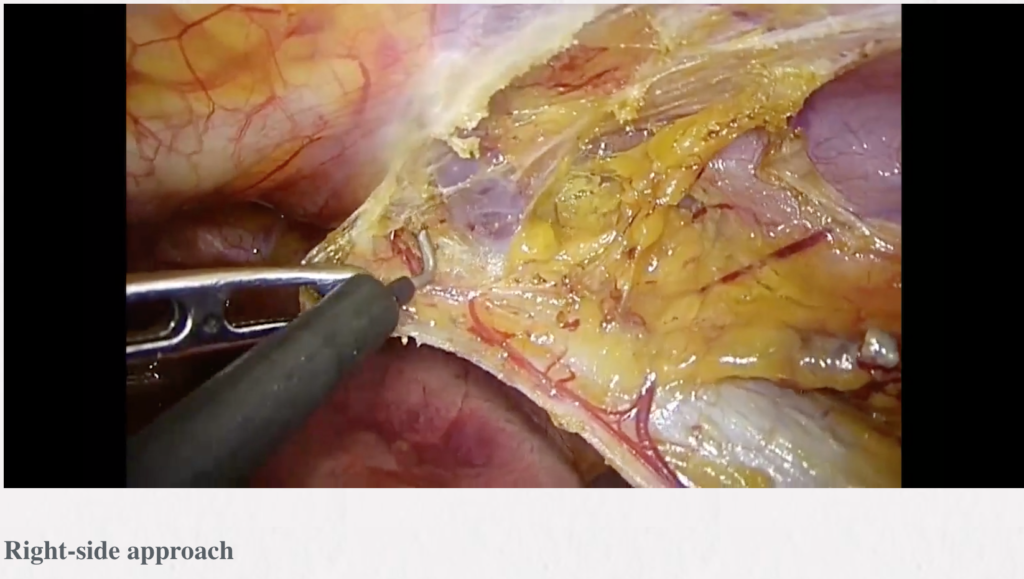
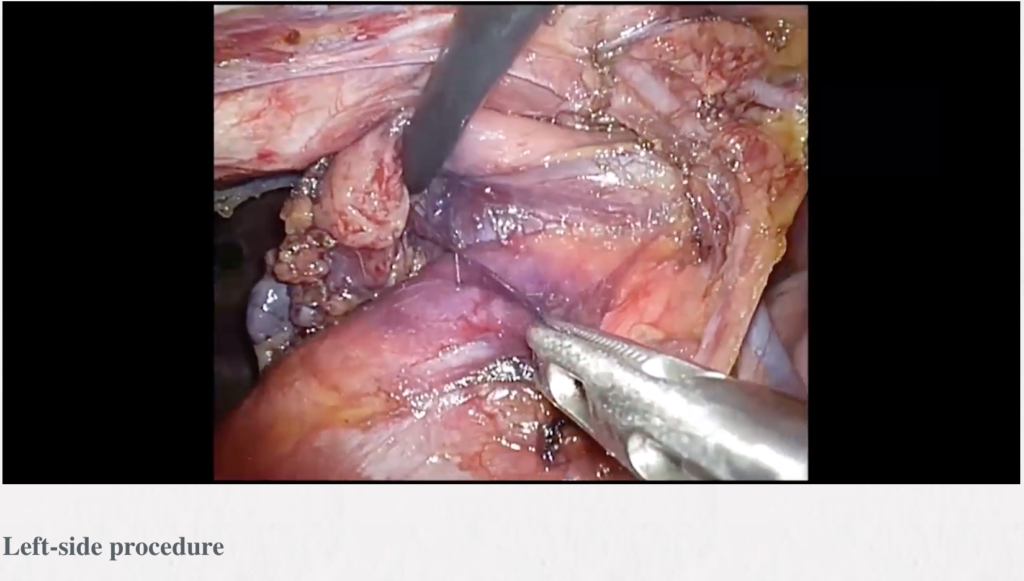
Video-assisted thoracic surgery thymectomy: a left-sided approach
Marcelo Jimenez, Maria Teresa Gomez-Hernandez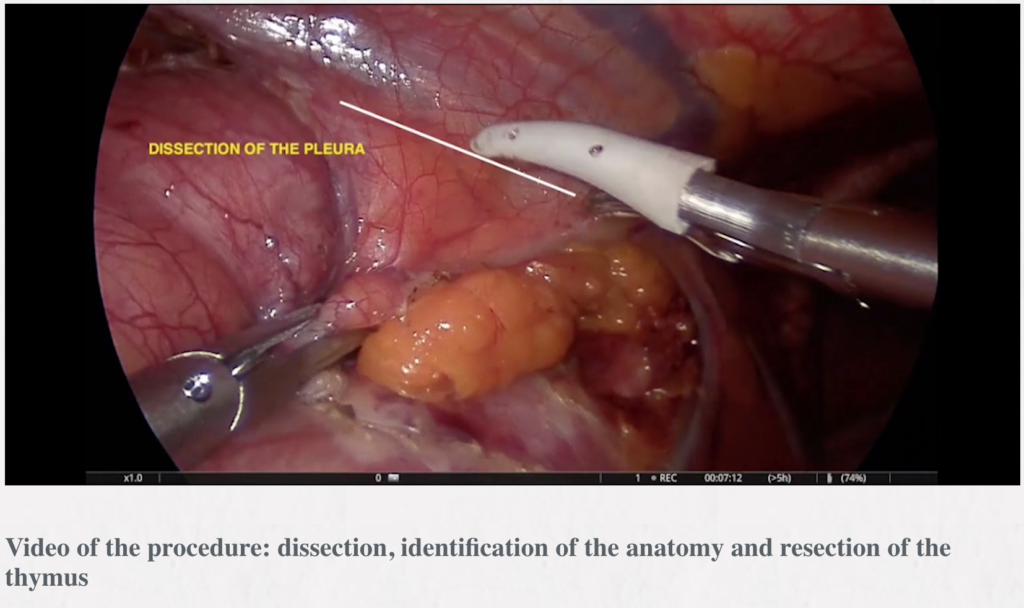
Department of Thoracic Surgery, Salamanca University Hospital, Salamanca, Spain
Abstract: We describe the left approach for thymectomy, which is currently our preferred approach. The left sided approach allows an excellent visualization of the aortopulmonary window where some thymic tissue can be located.
 VATS thymectomy—bilateral approach for extended resection
VATS thymectomy—bilateral approach for extended resection
Meinoshin Okumura, Yasushi Shintani, Soichiro Funaki, Ryu Kanzaki, Naoko Ose, Masato Minami
Department of General Thoracic Surgery (L-5), Osaka University Graduate School of Medicine, 2-2 Yamada-oka Suita-City Osaka 565-0871, Japan
 Abstract: Various bilateral VATS thymectomy procedures were introduced in the 1990’s, of which a bilateral VATS extended thymectomy has an advantage of confirming the bilateral phrenic nerves and seems to be the most conventional method in use. Soon after introduction of the method, an anterior cervical incision approach was added, because peri-thymic tissues are thought to reside mostly around the upper poles of the thymus. Studies have shown that significant amounts of thymic and peri-thymic tissues are left behind without use of a cervical incision. Later, several additional techniques, including elevation of the sternum, division of the right internal thoracic vein, and CO2 insufflation, served to make a cervical incision unnecessary and also providing a cosmetic advantage. Nevertheless, this procedure is still thought to be more invasive than a unilateral approach in terms of longer procedure time and bilateral thoracic incision. Recently, a uniportal bilateral approach was reported and advancement to a reduced port might be a means for achieving a less invasive approach for a bilateral VATS extended thymectomy.
Abstract: Various bilateral VATS thymectomy procedures were introduced in the 1990’s, of which a bilateral VATS extended thymectomy has an advantage of confirming the bilateral phrenic nerves and seems to be the most conventional method in use. Soon after introduction of the method, an anterior cervical incision approach was added, because peri-thymic tissues are thought to reside mostly around the upper poles of the thymus. Studies have shown that significant amounts of thymic and peri-thymic tissues are left behind without use of a cervical incision. Later, several additional techniques, including elevation of the sternum, division of the right internal thoracic vein, and CO2 insufflation, served to make a cervical incision unnecessary and also providing a cosmetic advantage. Nevertheless, this procedure is still thought to be more invasive than a unilateral approach in terms of longer procedure time and bilateral thoracic incision. Recently, a uniportal bilateral approach was reported and advancement to a reduced port might be a means for achieving a less invasive approach for a bilateral VATS extended thymectomy.
Transcervical thymectomy
Marcin Zieliński1, Mariusz Rybak1*, Katarzyna Solarczyk-Bombik1, Michal Wilkojc1, Wojciech Czajkowski1, Sylweriusz Kosinski2, Edward Fryzlewicz2, Tomasz Nabialek2, Malgorzata Szolkowska3, Juliusz Pankowski4
1Department of the Thoracic Surgery, 2Department the Anesthesiology and Intensive Care, Pulmonary Hospital, Zakopane, Poland; 3Department of Pathology of the Tuberculosis Institute, Warsaw, Poland; 4Department of Pathology, Pulmonary Hospital, Zakopane, Poland
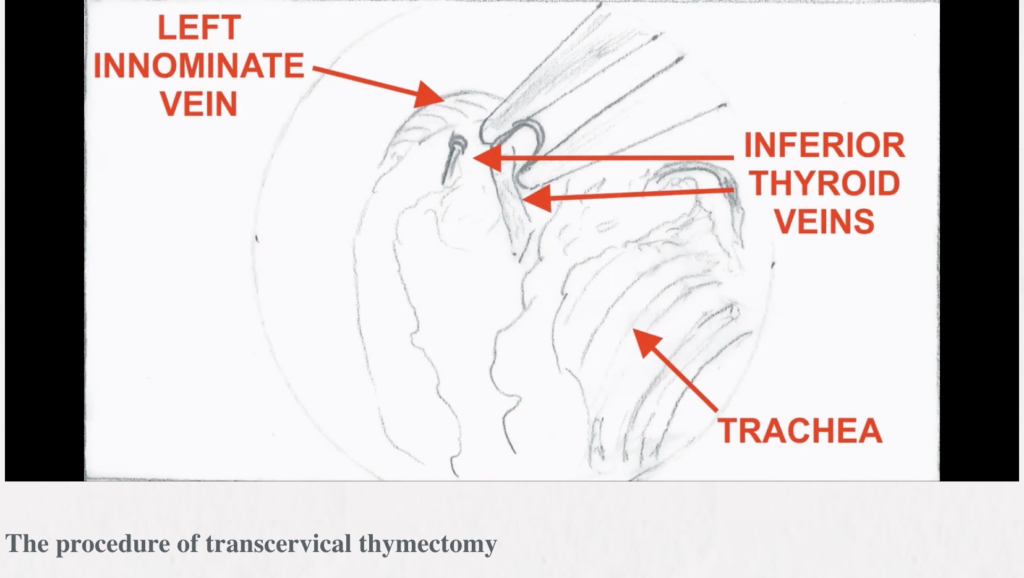 Background: The aim of this article is to describe the technique of minimally invasive extended thymectomy performed through the transcervical video-thoracoscopic (VATS) approach with elevation of the sternum for the thymic tumors with/without myasthenia gravis (MG).
Background: The aim of this article is to describe the technique of minimally invasive extended thymectomy performed through the transcervical video-thoracoscopic (VATS) approach with elevation of the sternum for the thymic tumors with/without myasthenia gravis (MG).
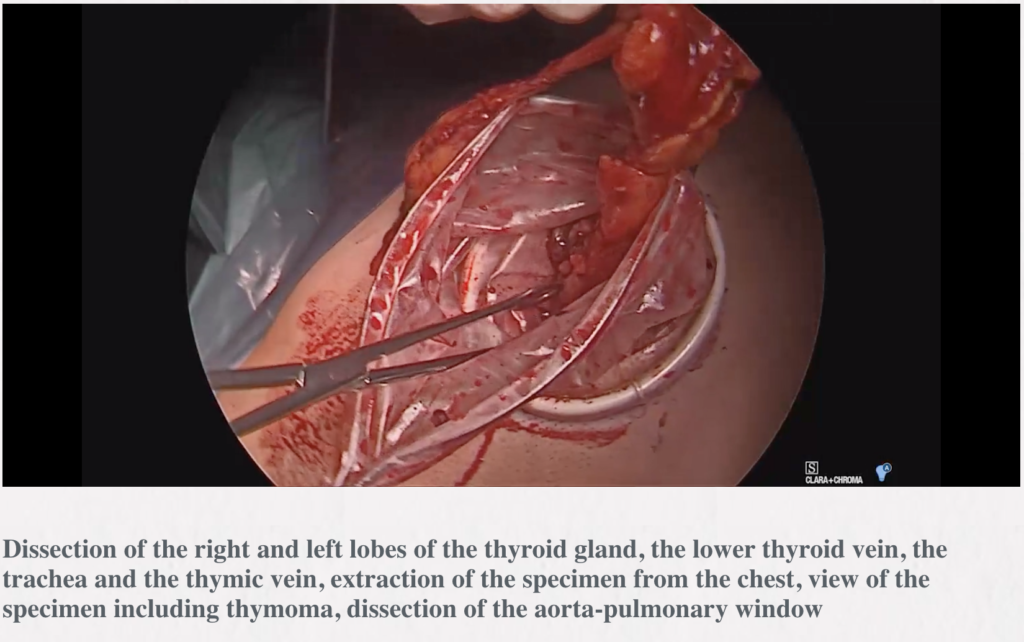
Methods: The operation is done through the collar incision in the neck of a length of 4–8 cm. To facilitate an access to the mediastinum a one-tooth hook connected to the Zakopane bar (Aesculap-Chifa, Nowy Tomysl, Poland) is inserted under the sternal notch for elevation of the sternum. Careful anatomical dissection of the structures of the lower neck region is done with preservation from injury of the thyroid gland, the parathyroid glands and both laryngeal recurrent nerves. The thymus gland is resected en-bloc with the surrounding fatty tissue of the lower neck and the anterior superior mediastinum. The blood vessels supplying the thymus are secured and divided—these are inferior thyroid veins and the thymic veins. For better control, a video-thoracoscope (VATS) is inserted to the mediastinum through the cervical incision. The lowers poles of the thymus are separated from the pericardium and the specimen is removed. Usually, the right lower pole is dissected first and the left lower pole is managed during further dissection of the aortopulmonary window is a difficult, but very important part of transcervical thymectomy.
Results: There were 18 patients (2 for MG with associated thymic tumors and 16 for the tumors/cysts of the anterior mediastinum without MG) in the period 1/1/2009 to 31/12/2017. The morbidity was 5.6%, with no mortality. The mean time of the procedure was 105.4 min (45–150 min).
Conclusions: The transcervical approach combined with VATS and lifting of the sternum facilitates thymectomy in case of small thymic tumors with/without MG. This technique is more difficult and less extensive that subxiphoid thymectomy.
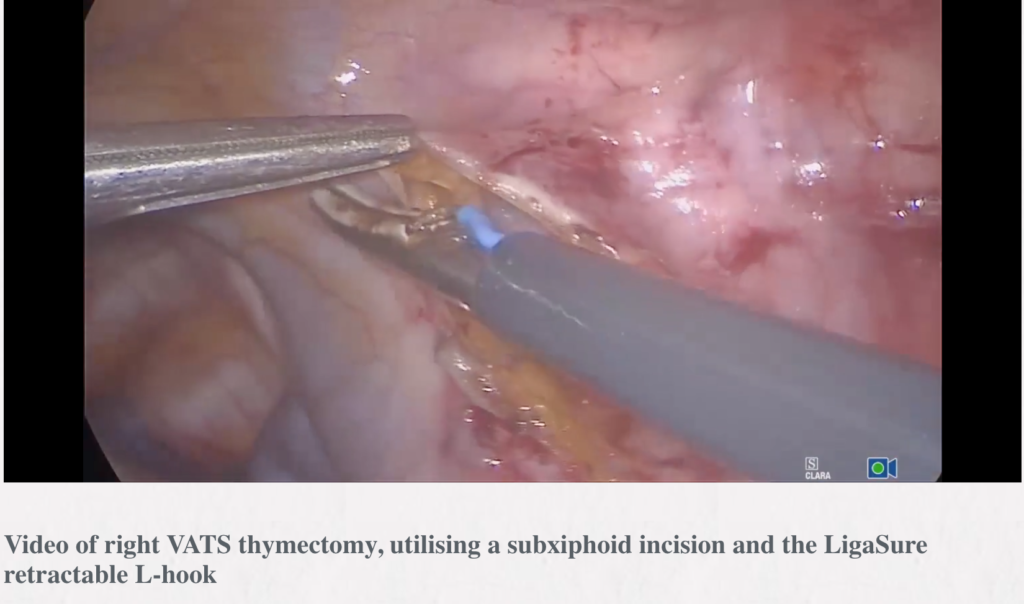 Right VATS thymectomy, utilising a subxiphoid incision and the LigaSure retractable L-hook
Right VATS thymectomy, utilising a subxiphoid incision and the LigaSure retractable L-hook
Joel Dunning1, Marco Nardini1, Ehab Bishay2
1Department of Thoracic Surgery, James Cook University Hospital, Middlesbrough, UK; 2Department of Thoracic Surgery, Birmingham Heartlands Hospital, Birmingham, UK
Abstract: We describe a technique of right sided video-assisted thoracoscopic surgery (VATS) thymectomy in a lady who had a large 7 cm mass which was adherent to the pericardium, extended into the superior poles of the thymus and had adhesions to the lung bilaterally. We utilized 3 mm × 5 mm ports from the right-hand side and a 12 mm subxiphoid incision which was used to retrieve the tumour at the end of the case. Due to the bulky nature of the tumour we also added a 5 mm port to the left chest to visualize the left phrenic nerve towards the end of the case. The pericardium is widely excised in this case as the tumour is adherent to it. The LigaSure L-hook is demonstrated which was particularly useful in this case. This device can grasp, blunt dissect, cut and seal as usual like any other LigaSure, but there is a switch that can retract the LigaSure back and advance a hook diathermy without removing the instrument from the chest. We hope this video and description demonstrates that endoscopic thymectomy is safe and feasible even in more difficult cases and provides the same completeness of resection as open surgery.
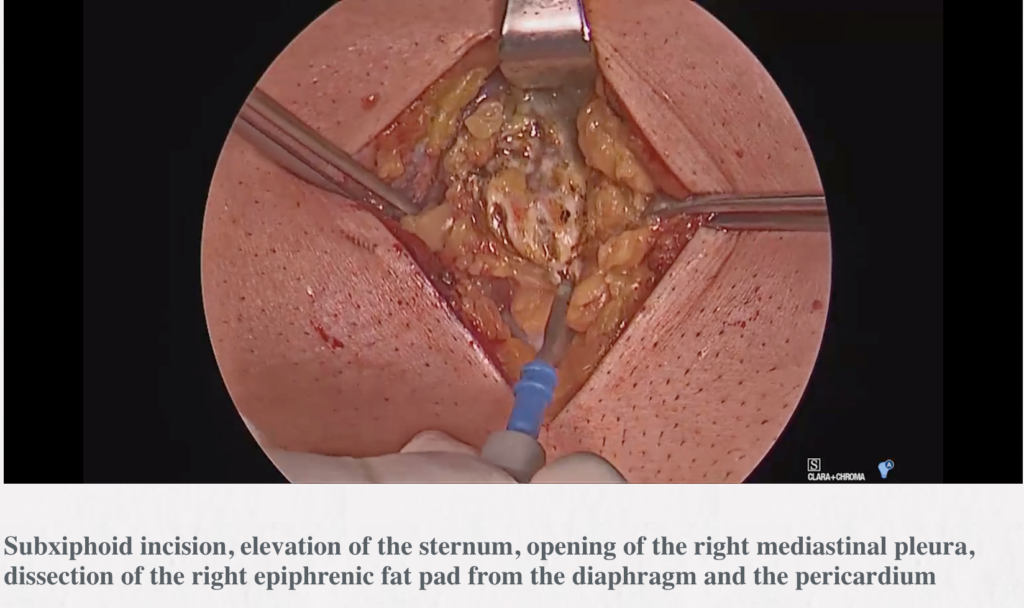 Video-assisted thoracic surgery thymectomy: subxiphoid approach
Video-assisted thoracic surgery thymectomy: subxiphoid approach
Marcin Zieliński1, Pawel Gwozdz1, Katarzyna Solarczyk-Bombik1, Michal Wilkojc1, Wojciech Czajkowski1, Sylweriusz Kosinski2, Edward Fryzlewicz2, Tomasz Nabialek2, Malgorzata Szolkowska3, Juliusz Pankowski4
1Department of Thoracic Surgery, 2Department of Anesthesiology and Intensive Care, Pulmonary Hospital, Zakopane, Poland; 3Department of Pathology, Tuberculosis Institute, Warsaw, Poland; 4Department of Pathology, Pulmonary Hospital, Zakopane, Poland
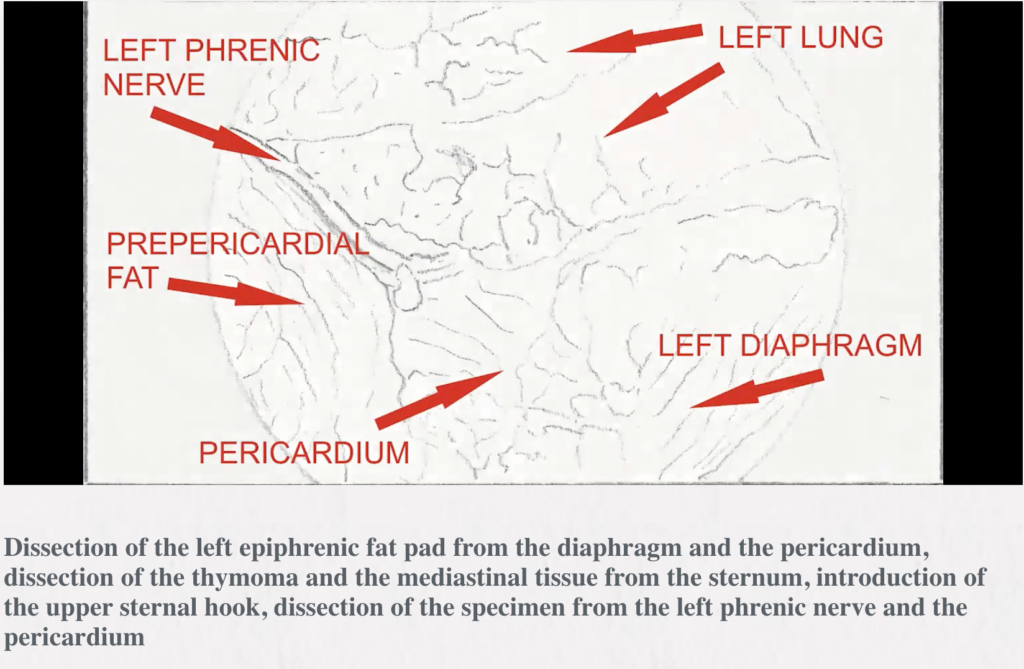 Background: To describe the use of the subxiphoid approach for thymectomy and to present a variant of the technique of minimally invasive extended thymectomy for thymoma or myasthenia gravis (MG) without thymoma done via a sole (uniportal) subxiphoid incision with aid of the sternal lifting.
Background: To describe the use of the subxiphoid approach for thymectomy and to present a variant of the technique of minimally invasive extended thymectomy for thymoma or myasthenia gravis (MG) without thymoma done via a sole (uniportal) subxiphoid incision with aid of the sternal lifting.
Methods: The infrasternal (subxiphoid) technique was used. The whole specimen containing the thymus surrounded by the right and left mediastinal pleural sheets and the fat of the anterior mediastinum and the lower neck region was resected en bloc through the incision made above the xiphoid process for insertion of a videothoracoscope [video-assisted thoracic surgery (VATS)] and, finally for introduction of chest drains. The sternum was lifted by two hooks attached to the Zakopane bar (B.Braun, Aesculap-Chifa, Nowy Tomysl, Poland). The lower hook was elevating the lower sternal angle and the upper hook was inserted through a puncture made above the sternal notch while the major mediastinal structures were pressed down toward the spine to avoid injury.
Results: The en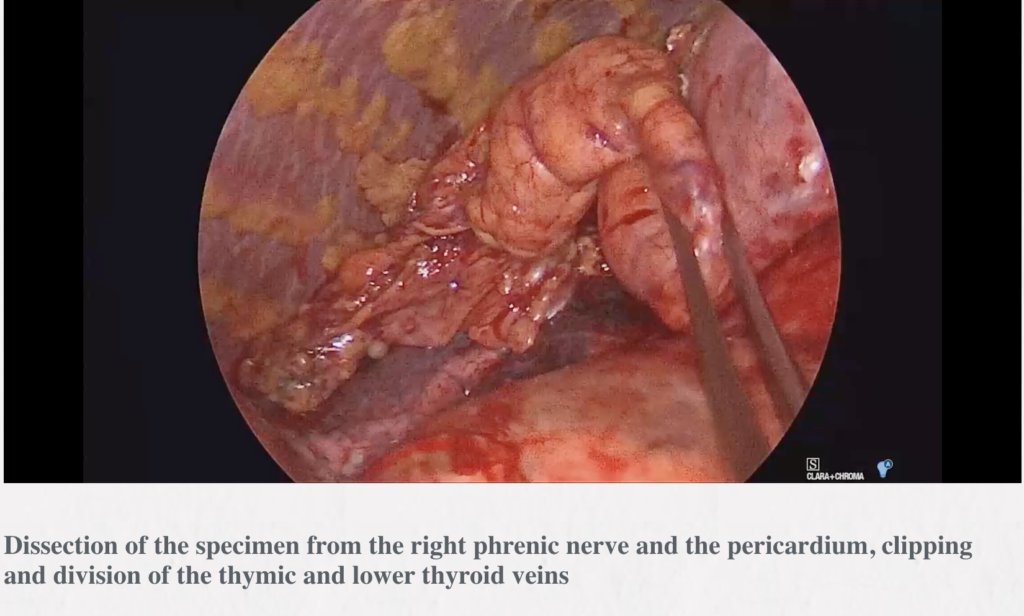 tire group of patients in whom the subxiphoid approach was used for thymectomy included 611 patients, overall (80 patients with thymomas, 516 patients with MG without thymoma and 15 patients with repeated thymectomy) operated on from Sep 2000 to Sep 2017. There were 5 uniportal subxiphoid-VATS extended thymectomies (for non-thymomatous MG in 2 patients and for thymic tumors in 2 patients). The mean time of the operation 118.5 min (range, 85–130 min). For the whole group of 611 patients there was no mortality and less than 5% morbidity. The complete remission rate 53.1% for the transcervical-subxiphoid-VATS maximal thymectomy approach for non-thymomatous MG was reported.
tire group of patients in whom the subxiphoid approach was used for thymectomy included 611 patients, overall (80 patients with thymomas, 516 patients with MG without thymoma and 15 patients with repeated thymectomy) operated on from Sep 2000 to Sep 2017. There were 5 uniportal subxiphoid-VATS extended thymectomies (for non-thymomatous MG in 2 patients and for thymic tumors in 2 patients). The mean time of the operation 118.5 min (range, 85–130 min). For the whole group of 611 patients there was no mortality and less than 5% morbidity. The complete remission rate 53.1% for the transcervical-subxiphoid-VATS maximal thymectomy approach for non-thymomatous MG was reported.
Conclusions: The subxiphoid uniportal incision with sternal lifting facilitates performance of extended thymectomy for thymomas or MG without thymoma.